Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
About this information
This information is for you if you want to know more about bleeding and/or pain in the first 3 months of pregnancy. It may be helpful if you are a relative or friend of someone who has bleeding and/or pain in early pregnancy.
What does vaginal bleeding and pain mean for me?
Vaginal bleeding and/or cramping pain in the early stages of pregnancy are common and do not always mean that there is a problem. However, bleeding and/or pain can be a warning sign of a miscarriage or, less commonly, of other complications of early pregnancy.
What should I do if I have bleeding and/or pain in the first 3 months?
If you have any bleeding and/or pain, you can get medical help and advice from:
What will happen when I attend hospital?
You will be asked about your symptoms and the date of your last period. You will also be asked about previous pregnancies and your general health. You may need to have:
You should be offered a chaperone (someone to accompany you) for a vaginal examination and a transvaginal scan. You may also wish to bring someone to support you during your examination or scan.
What could be causing bleeding and/or pain at this stage of pregnancy?
A threatened miscarriageIf you have had bleeding and/or pain but your ultrasound scan confirms that your pregnancy is progressing normally, this is known as a threatened miscarriage. Many women who bleed at this stage of pregnancy go on to have a healthy baby. You may be offered a follow-up scan.
An early miscarriageUnfortunately, bleeding and/or pain in early pregnancy can mean that you have had or are having a miscarriage. Sadly, early miscarriages are common. In the first 3 months, one in five women will have a miscarriage, for no apparent reason, following a positive pregnancy test.
However, most miscarriages occur as a one-off event and there is a good chance of having a successful pregnancy in the future. For further information on miscarriage, see the RCOG patient information Early miscarriage (www.rcog.org.uk/en/patients/patient-leaflets/early-miscarriage).
An ectopic pregnancyWhen a pregnancy starts to grow outside the womb, it is called an ectopic pregnancy. In the UK, one in 90 pregnancies is ectopic. Your symptoms, scan findings and blood tests might lead to suspicion that you have an ectopic pregnancy.
An ectopic pregnancy can pose a risk to your health. If this is suspected or confirmed, you may be advised to stay in hospital. For further information, see the RCOG patient information An ectopic pregnancy (www. rcog.org.uk/en/patients/patient-leaflets/ectopic-pregnancy).
A molar pregnancyA molar pregnancy is an uncommon condition where the placenta is abnormal and the pregnancy does not develop properly. It affects only one in 700 pregnancies. A molar pregnancy is usually diagnosed when you have an ultrasound scan. For further information, see the RCOG patient information Gestational trophoblastic disease (www.rcog.org.uk/en/patients/patient-leaflets/gestational-trophoblastic-disease-gtd).
A pregnancy of unknown location (PUL)If you have a positive pregnancy test and your pregnancy cannot be seen clearly on ultrasound scan, it is known as a pregnancy of unknown location (PUL).
Reasons for this may be:
I have been told that I have a PUL – what happens next?
It is important that you are followed up to get a diagnosis and to confirm whether your pregnancy is continuing or not. You will be given an appointment to attend your early pregnancy unit for follow-up.
You are likely to be asked to come every 2–3 days for a blood test to check the level of your pregnancy hormone (βhCG). The results should help show where the pregnancy is developing. They will also help to guide your follow-up:
You may also be booked for another ultrasound scan, usually within 1–2 weeks. If an ectopic pregnancy is suspected, a member of staff may contact you with your results and give you advice.
This uncertainty will be difficult but it often takes time to come to the right diagnosis. Sometimes this is reached within a few days but it may take up to 2 weeks. The team looking after you will discuss your options at each step.
What symptoms should I be aware of while I am being monitored?
It is important that you are aware of the signs of an ectopic pregnancy (below) and that you seek urgent medical help if you have any of them. Fortunately, most women with a PUL do not have an ectopic pregnancy.
What are the disadvantages of VBAC?
Successful VBAC has fewer complications than ERCS. If you do have a successful vaginal birth:
Contact your Early Pregnancy Assessment Service or A&E department immediately if you have any of the following:
Key points
Further information
Association of Early Pregnancy Units (AEPU): www.earlypregnancy.org.uk
Miscarriage Association: www.miscarriageassociation.org.uk
National Institute for Health and Care Excellence (NICE): Ectopic Pregnancy and Miscarriage: www.nice.org.uk/ guidance/cg154/ifp/chapter/About-this-information
NHS 111 service: www.nhs.uk/NHSEngland/AboutNHSservices/Emergencyandurgentcareservices/Pages/ NHS-111.aspx
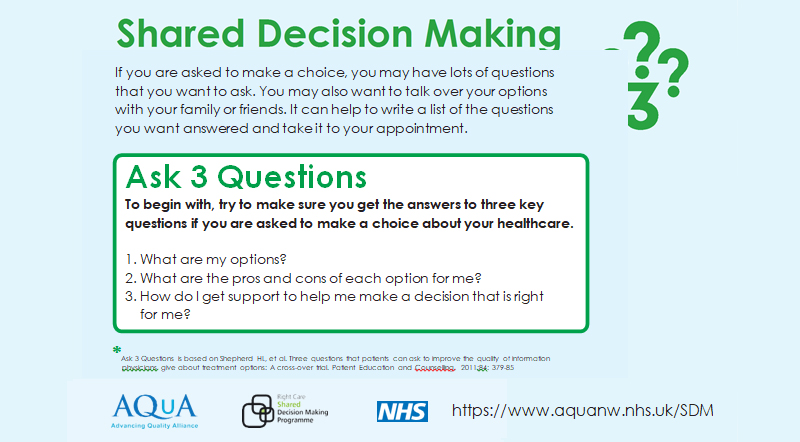
Making a choice
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the NICE Guideline Ectopic Pregnancy and Miscarriage: Diagnosis and Initial Management, which you can find online at: www.nice.org.uk/guidance/CG154.
This leaflet was reviewed before publication by women attending clinics in Liverpool, Chester, Prescot, Wrexham and Inverness, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
The RCOG produces guidelines as an educational aid to good clinical practice. They present recognised methods and techniques of clinical practice, based on published evidence, for consideration by obstetricians and gynaecologists and other relevant health professionals. This means that RCOG guidelines are unlike protocols or guidelines issued by employers, as they are not intended to be prescriptive directions defining a single course of management.
A glossary of all medical terms is available on the RCOG website at: www.rcog.org.uk/en/patients/medical-terms.