Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
About this information
This information is for you if you want to know more about polycystic ovary syndrome (PCOS). It may be helpful if you are a patient, relative or friend of someone who has PCOS.
What is polycystic ovary syndrome?
PCOS is a condition that can affect your periods, fertility, hormones and aspects of your appearance. It can also affect your long-term health. Estimates of how many women it affects vary widely from 2 to 26 in every 100 women. This information is about the effects on your long-term health and does not cover specific treatment options for PCOS.
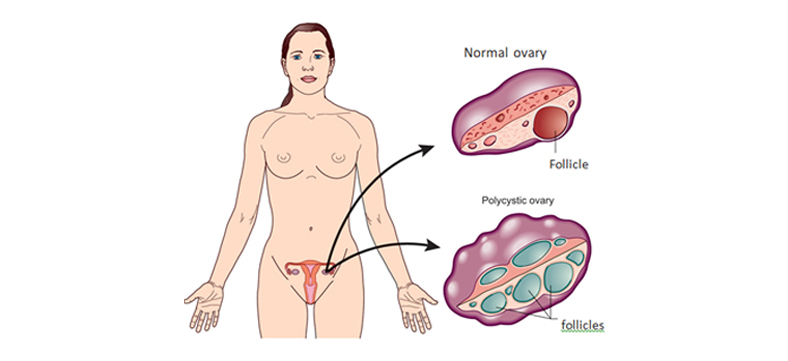
Having polycystic ovaries does not necessarily mean that you have PCOS. Women with PCOS have symptoms as well as polycystic ovaries.
What are the symptoms of PCOS?
The symptoms of PCOS include:
Depression and psychological problems can also result from having PCOS.
The symptoms vary from woman to woman. Some women have very few mild symptoms, while others are affected more severely by a wider range of symptoms.
PCOS is a cause of fertility problems in women. For further information see Fertility: Assessment and Treatment for People with Fertility Problems, which is produced by the National Institute for Health and Care Excellence (NICE) and is available at: www.nice.org.uk/guidance/cg156.
You may still become pregnant even if you do not have periods. If you do not want to become pregnant, you should seek advice from your GP about contraception.
What causes PCOS?
The cause of PCOS is not yet known but it often runs in families. If any of your relatives (mother, aunts, sisters) are affected with PCOS, your risk of developing PCOS may be increased.
The symptoms are related to abnormal hormone levels:
How is PCOS diagnosed?
Having polycystic ovaries does not mean you have PCOS.
Women with PCOS often have symptoms that come and go, particularly if their weight goes up and down. This can make it a difficult condition to diagnose, which means it may take a while to get a diagnosis.
A diagnosis is made when you have any two of the following:
When a diagnosis is made, you may be referred to a gynaecologist (a doctor who specialises in caring for a woman’s reproductive system) or an endocrinologist (a doctor who specialises in the hormonal system).
What could PCOS mean for my long-term health?
If you have PCOS, you are at greater risk of developing the long-term health problems discussed below.
Insulin resistance and diabetes If your blood glucose does not stay normal, this can lead to diabetes. One or two in every ten women with PCOS go on to develop diabetes at some point. If the diabetes is untreated, this can cause damage to organs in the body.
If you have PCOS, your risk of developing diabetes is increased further if you:
If you are diagnosed with diabetes, you will be given advice about your diet and may be prescribed tablets or insulin injections.
High blood pressure Women with PCOS tend to have high blood pressure, which is likely to be related to insulin resistance and to being overweight rather than to the PCOS itself. High blood pressure can lead to heart problems and should be treated.
If your scan suggests that you have a complex cyst, you might be offered blood tests, which can help to determine what type of cyst it is. You do not need blood tests if a simple cyst is diagnosed.
Cancer If you have fewer than three periods a year, the lining of the womb (endometrium) can thicken and this may lead to endometrial cancer in a small number of women.
There are various ways to protect the lining of the womb using the hormone progestogen. Your doctor will discuss the options with you. This may include a five-day course of progestogen tablets used every three or four months, taking a contraceptive pill or using the intrauterine contraceptive system (Mirena®). The options will depend on whether you are trying for a baby.
PCOS does not increase your chance of breast or ovarian cancer.
Depression and mood swings The symptoms of PCOS may affect how you see yourself and how you think others see you. It can lower your self-esteem.
Snoring and daytime drowsiness PCOS can lead to fatigue or sleepiness during the day. It is also associated with snoring.
What can I do to reduce long-term health risks?
Have a healthy lifestyle The main ways to reduce your overall risk of long-term health problems are to:
Your GP or practice nurse can provide you with full information on eating a healthy diet and exercise.
You should aim to keep your weight to a level that is normal. BMI is the measurement of weight in relation to height and you should aim to keep your BMI between 19 and 25. To calculate your BMI, follow this link: www.nhs.uk/Tools/Pages/Healthyweightcalculator.aspx.
If you are overweight, it would be helpful to lose weight and maintain your weight at this new level. If your BMI is more than 30, discuss ways of losing weight, including weight-reducing drugs, with your GP, practice nurse or pharmacist.
The benefits of losing weight include:
You only have to lose a small amount of weight to make a difference to your symptoms and your health.
There is no strong evidence that PCOS by itself can cause you to gain weight or makes losing weight difficult. Many women find great benefit from support groups such as Verity (www.verity-pcos.org.uk).
Have regular health checks
Once you have a diagnosis of PCOS, you will be monitored to check for any early signs of health problems:
Is there a cure?
There is no cure for PCOS. Medical treatments aim to manage and reduce the symptoms or consequences of having PCOS. Medication alone has not been shown to be any better than healthy lifestyle changes (weight loss and exercise).
Many women with PCOS successfully manage their symptoms and long-term health risks without medical intervention. They do this by eating a healthy diet, exercising regularly and maintaining a healthy lifestyle.
Sources and acknowledgements