Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
About this information
This information is for you if you want to know more about being pregnant with a small baby. You may find it helpful if you are pregnant and have been told your unborn baby may be small. If you are a partner, relative or friend of someone who is in this situation, you may also find it helpful.
It tells you:
This information is not for women who are pregnant with more than one baby.
What is meant by a small baby during pregnancy?
An unborn baby is small if, at that stage of pregnancy, his or her size or estimated weight on scan is in the lowest 10% of babies. This means the smallest ten out of every 100 babies.
What affects my baby’s birthweight?
Your baby’s weight is affected by many things, including:
What could cause my baby to be small?
Your baby could be small because of a combination of the factors above. If this is the case, your baby is likely to be healthy because he or she is meant to be small.
However, sometimes babies are small because they do not grow as well as expected. This is called being ‘growth restricted’. Causes of growth restriction include:
What increases the risk of my baby not growing well?
Lifestyle choices such as smoking, using cocaine, over-exercising or not eating healthily are all linked to an increased chance of the baby being growth restricted.
You are more likely to have a baby that is growth restricted if you are over 40 or have high blood pressure, kidney problems or diabetes complications. Having lost a baby late in pregnancy or having had a small baby in the past also increases your risk.
Heavy vaginal bleeding, especially in the second half of pregnancy, can also affect the way your baby grows.
Can I do anything to reduce the risk?
Some of these risks cannot be changed, but some can:
What does being small mean for my baby?
If your baby is small but healthy, he or she is not at increased risk of complications.
If your baby is growth restricted, there is an increased risk of stillbirth (the baby dying in the womb), serious illness and dying shortly after birth. The earlier in pregnancy and the more severely your baby’s growth is affected, the more likely it is that your baby will have a poor outcome. Babies whose growth is only affected later in pregnancy have a better outcome.
Most babies affected by infection or by developmental or genetic problems have severe growth restriction and are usually detected early.
Once your healthcare team has identified that your baby is small, you will be offered extra monitoring to keep an eye on your baby’s growth and wellbeing. You are likely to be advised to have your baby early to be as certain as possible that your baby will be born healthy.
How will I know if I am having a small baby?
Your midwife or obstetrician should assess your risk of having a small baby in early pregnancy:
If my baby is small or not growing, what other tests may I be offered?
You may have the following tests to check your baby’s wellbeing:
You may be referred to a fetal medicine specialist for more frequent and detailed scans if the umbilical artery Doppler test is abnormal.
When is the best time for my baby to be born?
This will depend on how affected your baby’s growth appears to be, and on the Doppler measurements. The scans will help your team decide whether it is better for your baby to be born early or safer for you and your baby to continue your pregnancy longer. If your baby is growing and the Doppler tests are normal, it is usually best to wait until you are at least 37 weeks pregnant.
Is there any other treatment I should have?
Depending on the timing of birth and the way you are going to have your baby, you may be offered a course of corticosteroids over a 24–48 hour period. This is to help your baby’s development and reduce the chance of breathing problems after birth. You can find out more about this from the RCOG patient information Corticosteroids in pregnancy to reduce complications from being born prematurely: information for you, which is available at: www.rcog.org.uk/womens-health/clinical-guidance/corticosteroids.
How will I have my baby?
If there are no other complications, you may be able to have a vaginal birth. Your baby will be monitored closely during labour. However, if the umbilical artery Doppler measurements are abnormal, your doctor may recommend that your baby be born by caesarean section.
If you go into labour, if your waters have broken or if you have had any bleeding before the date that you have been advised to have your baby, you should attend hospital straight away.
Where should I have my baby?
You will be advised to have your baby in a hospital where there is a neonatal unit (special care baby unit).
Whether your baby will need to be looked after in the neonatal unit will depend on how small your baby is and at what stage of pregnancy your baby is born. You should have an opportunity to talk to one of the neonatal team if it is likely that your baby will need special care. You and your partner may also wish to visit the neonatal unit if this is the case.
What to do if I have concerns or further questions
Talk to your midwife, who should be able to help. You can also ask to speak to your team of doctors and midwives at your maternity unit.
Further information aimed at healthcare professionals is also available in the RCOG Green-top Guideline No. 31, The Investigation and Management of the Small-for-Gestational-Age Fetus, which is available at: www. rcog.org.uk/womens-health/investigation-and-management-small-gestational-age-fetus-green-top-31.
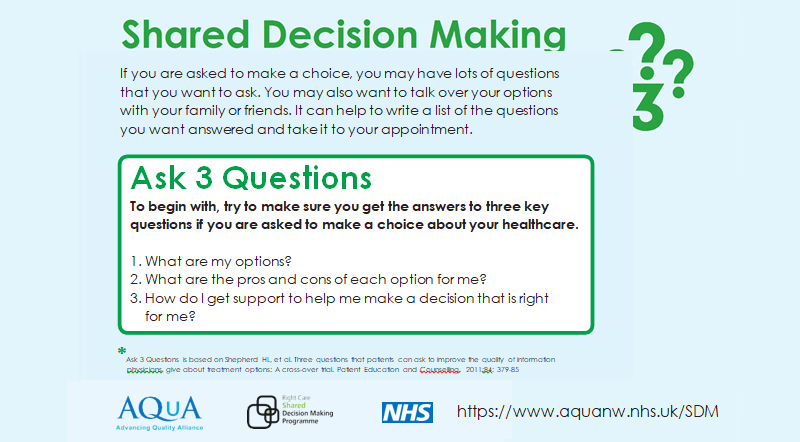
Making a choice
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Guideline No. 31, The Investigation and Management of the Small-for-Gestational-Age Fetus, which is available at: www.rcog.org.uk/womens-health/investigation-and-management-small-gestational-age-fetus- green-top-31. The guideline contains a full list of the sources of evidence we have used.
The RCOG produces guidelines as an educational aid to good clinical practice. They present recognised methods and techniques of clinical practice, based on published evidence, for consideration by obstetricians and gynaecologists and other relevant health professionals. This means that RCOG guidelines are unlike protocols or guidelines issued by employers, as they are not intended to be prescriptive directions defining a single course of management.
This leaflet was reviewed before publication by women attending clinics in Belfast, Glasgow, Kirkcaldy, Newcastle and Birmingham.
A glossary of all medical terms is available on the RCOG website at: www.rcog.org.uk/womens-health/patient- information/medical-terms-explained.