Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
What is pelvic organ prolapse?
The organs within a woman’s pelvis (uterus, bladder and rectum) are normally held in place by ligaments and muscles known as the pelvic floor. If these support structures are weakened by overstretching, the pelvic organs can bulge (prolapse) from their natural position into the vagina. When this happens it is known as pelvic organ prolapse. Sometimes a prolapse may be large enough to protrude outside the vagina.
This information is for you if you have been told that you have or if you think you may have a prolapse into the vagina. It explains what can cause prolapse and the various options for treatment.
It aims to help you understand the condition better to help you and your healthcare team make the best decisions about your care. It is not meant to replace advice from a doctor, nurse or physiotherapist about your own situation.
Key points
How common is pelvic organ prolapse?
It is difficult to know exactly how many women are affected by prolapse since many do not go to their doctor about it. However, it does appear to be very common, especially in older women. Half of women over 50 will have some symptoms of pelvic organ prolapse and by the age of 80 more than one in ten will have had surgery for prolapse.
Why does pelvic organ prolapse happen?
Often it is a combination of these factors that results in you having a prolapse.
What are the different types of prolapse?
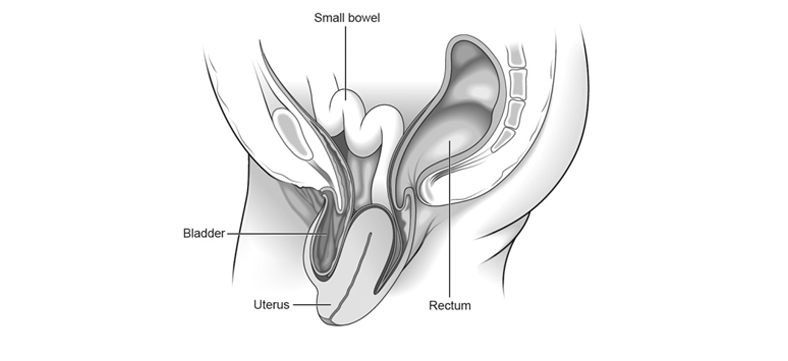
There are different types of prolapse depending on which organ is bulging into the vagina. The uterus, bladder, or rectum may be involved. It is common to have more than one type of prolapse at the same time.
Normal pelvic anatomy looks like this:
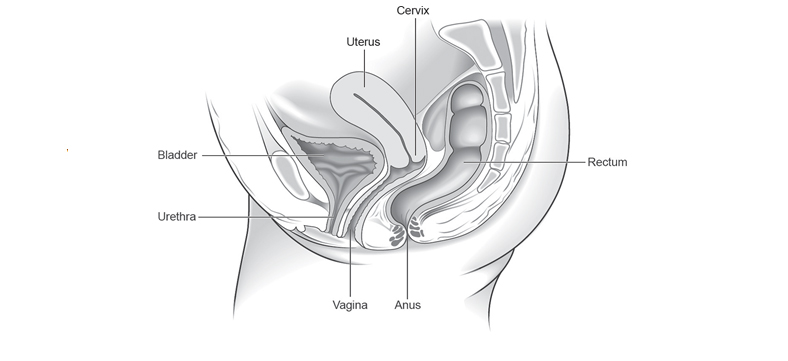
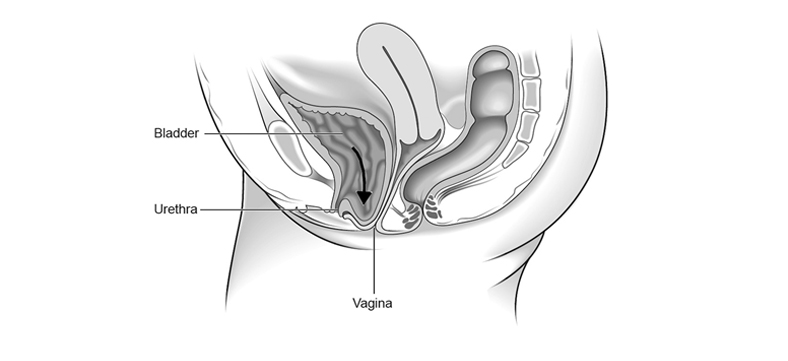
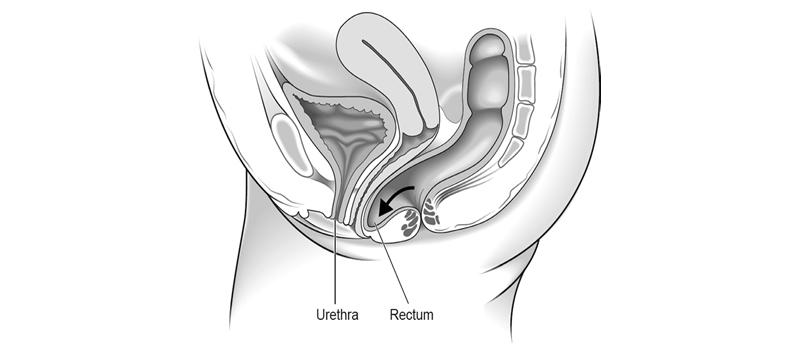
The most common types of prolapse are:
Anterior wall prolapse (cystocele) – when the bladder bulges into the front wall of the vagina.
Posterior wall prolapse (rectocele) – when the rectum bulges into the back wall of the vagina.
Uterine prolapse – when the uterus hangs down into the vagina. Eventually the uterus may protrude outside the body. This is called a procidentia or third-degree prolapse.
Vault prolapse – after a hysterectomy has been performed, the top (or vault) of the vagina may bulge down. This is called a vault prolapse. This happens to one in ten women who have had a hysterectomy to treat their original prolapse.
There are different degrees of prolapse depending on how far the organ(s) have bulged. It is important to distinguish between the various types and degrees of pelvic organ prolapse as their symptoms and treatment may differ.
What are the symptoms of pelvic organ prolapse?
Your symptoms will depend on the type and severity of your prolapse.
How is prolapse diagnosed?
A prolapse is diagnosed by performing a vaginal examination. Your doctor will usually insert a speculum (a plastic or metal instrument used to separate the walls of the vagina to show or reach the cervix) into the vagina to see exactly which organ(s) are prolapsing. You may be asked to lie on your left side with your knees drawn up slightly towards your chest in order to for this examination to be performed. You may also be examined standing up.
Will I need any tests?
You may have had a urine test to check for infection. If you have bladder symptoms, particularly if you leak when you cough or laugh, you may be referred for special bladder tests known as urodynamics. These are usually done in a hospital.
Do I have to have treatment?
No. If you only have a mild prolapse or have no symptoms from your prolapse, you may choose or be advised to take a ‘wait and see’ approach.
However, the following may ease your symptoms and stop your prolapse from becoming worse:
What are my options for treatment?
Your options for treatment will depend on the type of prolapse you have, how severe it is and your individual circumstances. Treatment options include the following.
Pessary
SurgeryThe aim of surgery is to relieve your symptoms while making sure your bladder and bowels work normally after the operation. If you are sexually active, every effort will be made to ensure that sex is comfortable afterwards.
Whether you choose to have surgery will depend on how severe your symptoms are and how your prolapse affects your daily life. You may want to consider surgery if other options have not adequately helped.
There are risks with any operation. These risks are higher if you are overweight or have medical problems. Your gynaecologist will discuss this with you so that you can decide whether you wish to go ahead with your operation.
If you plan to have children, you may choose to delay surgery until your family is complete. If you do undergo surgery, you may be advised to have a caesarean section if you become pregnant.
What are the different types of surgery for pelvic organ prolapse?
There are many different operations that can be performed to treat prolapse. Your gynaecologist will advise you which operation is best for you. This will depend on your type of prolapse and your symptoms, as well as your age, general health, wish to have sexual intercourse and whether or not you have completed your family.
If there is more than one choice, your gynaecologist will explain the pros and cons of each.
Surgery for prolapse is usually performed through the vagina but may involve a cut in your abdomen or keyhole surgery. If your gynaecologist is not able to offer the operation that best meets your needs, you may be referred to a specialist unit. New surgical techniques are being developed all the time. You should talk to your gynaecologist to find out whether there is anything new that might be more suitable for you.
Possible operations include:
It may be possible to treat urinary incontinence at the same time as surgery for prolapse and your doctor will discuss this with you if relevant.
Sometimes when you are relaxed under the anaesthetic, other areas of prolapse can become obvious. Your surgeon may request your consent to operate on those areas of prolapse as well. This should be fully discussed with you before your operation.
How successful is surgery for pelvic organ prolapse?
No operation can be guaranteed to cure your prolapse, but most offer a good chance of improving your symptoms. The benefits of some last longer than others.
About 25–30 out of 100 women having surgery for prolapse will develop another prolapse in the future. There is a higher chance of the prolapse returning if you are overweight, constipated, have a chronic cough or undertake heavy physical activities. Prolapse may occur in another part of the vagina and may need repair at a later date.
What might happen if I don’t have an operation?
Your problems may remain the same or get worse, or sometimes even improve over time. There is no way of confidently predicting this but an advanced prolapse cannot be expected to improve without a pessary or surgery. Prolapse is not life-threatening although it may affect the quality of your life. You can reconsider your options at any time.
Is there anything else I need to know?
The length of time you need to spend in hospital after the operation will vary depending on the type of operation and how quickly you recover, but will usually be no more than a few days. Generally speaking, you should avoid heavy lifting after surgery and avoid sexual intercourse for 6–8 weeks.
Further information
Recovering after your operation RCOG patient information on Return to Fitness: Recovering Well: www.rcog.org.uk/recovering-well.
Information for you after a pelvic-floor repair operation: www.rcog.org.uk/information-for-you-after-pelvic- floor-repair-operation.
Information for you after a vaginal hysterectomy: www.rcog.org.uk/information-for-you-after-a-vaginal- hysterectomy.
The use of mesh for prolapse RCOG statement on report commissioned by the MHRA on vaginal tape and mesh implants: www.rcog. org.uk/news/rcog-statement-report-commissioned-mhra-vaginal-tape-and-mesh-implants.
MHRA Information for patients: Vaginal mesh for pelvic organ prolapse: www.mhra.gov.uk/ Safetyinformation/Generalsafetyinformationandadvice/Product-specificinformationandadvice/Product- specificinformationandadvice–M–T/Vaginalmeshforpelvicorganprolapse/Informationforpatients/index.htm.
Sources and acknowledgements