Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
About this information
Finding out you are having twins, triplets or even quadruplets can be exciting, but it may also bring worries and concerns for you, your partner and family members. If you are expecting more than one baby, it is important that you are well prepared for the changes that will take place both during your pregnancy and after the babies’ birth.
This information is for you if you know you are carrying more than one baby. It tells you about:
This leaflet provides an overview of multiple pregnancy: it focuses mainly on twins but it is relevant to any pregnancy where more than one baby is expected. Further information and support is available from your midwife and obstetrician and from the multiple-pregnancy organisations listed at the end of the leaflet.
What is a multiple pregnancy?
A ‘multiple pregnancy’ is the term used when you are expecting two or more babies at the same time. It occurs in about one in 80 pregnancies. Fertility treatment increases the chances of multiple pregnancy.
What are the different kinds of multiple pregnancy?
At your early ultrasound scan which confirms whether you are carrying twins or triplets, it is important to find out the ‘chorionicity’ of your pregnancy. This is to help identify whether your babies share a placenta and it is important because babies who share a placenta have a higher risk of complications.
Twins can be:
Similarly, triplets can be trichorionic (each baby has a separate placenta and chorion), dichorionic (two of the three babies share a placenta and chorion and the third baby is separate), or monochorionic (all three babies share a placenta and chorion).
If your babies share a placenta, they are identical or ‘monozygotic’. Most babies who do not share a placenta are non-identical or ‘dizygotic’. However, it is possible for babies not sharing a placenta to be identical as well. This is because nearly a third of monozygotic or identical twins will each have their own placenta and hence will have the same appearance on ultrasound scans as the DCDA (non-identical or dizygotic) twins.
What does a multiple pregnancy mean for my babies and me?
Most women who have a multiple pregnancy have healthy pregnancies and healthy babies. However, complications are more common in multiple pregnancy and having extra care during your pregnancy including more ultrasound scans reduces these risks to you and your babies.
For you
Minor problems that many pregnant women experience, such as morning sickness, heartburn, swollen ankles, varicose veins, backache and tiredness, are more common in multiple pregnancies. They get better naturally after the babies are born.
Any problems that arise in any pregnancy are more common with twins and include:
For your babies
Prematurity
You are more likely to have your babies early if you are expecting twins or triplets:
Babies born earlier than 37 weeks of pregnancy have an increased risk of problems, particularly with breathing, feeding and infection. The earlier your babies are born, the more likely this is to be the case. They may need to be looked after in a neonatal unit. You will be supported to spend as much time as you can with them and you will be encouraged to breastfeed. For more information, see the RCOG patient information Premature labour (www.rcog.org.uk/en/patients/patient-leaflets/premature-labour).
Having a baby born early can be worrying and distressing for parents. Your babies are more likely to need special care after birth. Your doctor or midwife will be happy to talk to you about this and can give you information about support groups that you might find helpful.
Problems with growth
Having twins increases the chance of the placenta not working as well as it should. This can affect the babies’ growth and wellbeing.
Twin-to-twin transfusion syndrome (TTTS)
Twins sharing a placenta (monochorionic pregnancies) also share the blood supply. In around 15 in 100 monochorionic twin pregnancies, the blood flow may be unbalanced. We call this twin-to-twin transfusion syndrome (TTTS). One baby, the ‘donor’, receives too little blood and has a low blood pressure while the other baby, the ‘recipient’, receives too much blood and has a high blood pressure. You will be monitored with frequent scans for signs of TTTS. It can be mild and may not require any treatment, or it can be serious, in which case you will be offered treatment in a hospital with specialist expertise.
What extra care will I need during pregnancy?
You will be under the care of a specialist healthcare team and will be advised to have your babies in a consultant-led maternity unit that has a neonatal unit. Your team will usually include an obstetrician and a midwife who specialises in multiple pregnancies.
Having a multiple pregnancy means that you will need more visits to the antenatal clinic at your hospital. You will be offered extra ultrasound scans to monitor your babies’ growth more closely.
Can I still have screening for Down syndrome and other abnormalities?
Like all women, you will be offered a scan at about 12–14 weeks to screen for chromosomal conditions such as Down syndrome. Even in multiple pregnancies, blood tests taken at the same time can be combined with the scan results to assess the risk of one or both of your babies having a chromosome problem; for further information, refer to the UK National Screening Committee (www.gov.uk/topic/ population-screening-programmes/fetal-anomaly).
You will also be offered another scan at around 20 weeks to look at your babies’ development. The chance of these tests finding a problem is slightly higher than if you were pregnant with only one baby. Your specialist team will be able to offer you advice if the screening shows any problems with your pregnancy.
Key points
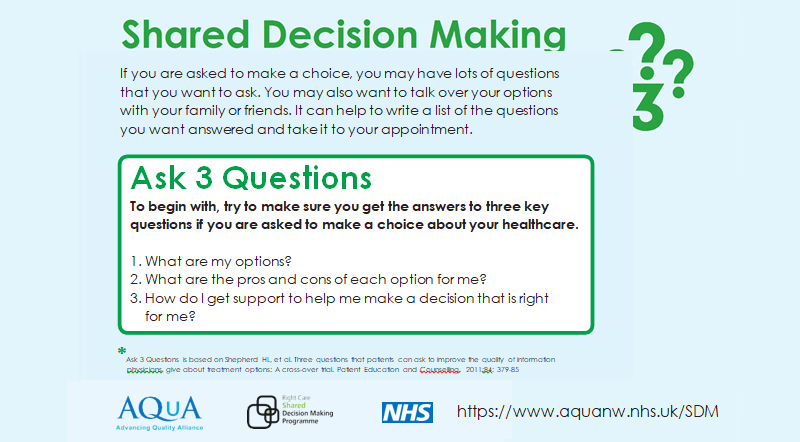
Making a choice
Further information
Twins & Multiple Births Association (TAMBA): www.tamba.org.uk
The Multiple Births Foundation: www.multiplebirths.org.uk
National Institute for Health and Care Excellence (NICE): Multiple pregnancy: Antenatal care for twin and triplet pregnancies: www.nice.org.uk/guidance/cg129/informationforpublic
UK National Screening Committee: www.gov.uk/topic/population-screening-programmes/fetal-anomaly
Sources and acknowledgements