Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
Who is this information for?
This information is for you if you want to know more about eating healthily in pregnancy. It also gives you advice about using vitamin supplements before you get pregnant and during pregnancy.
Healthy eating
Keeping healthy when you are having a baby depends on both the amount and the type of food you eat before you become pregnant and during your pregnancy. Simply being a correct weight for your height does not necessarily mean that you are eating healthily. Some foods are best avoided if you are planning to become pregnant or if you are already pregnant, as they may contain substances that could affect your unborn baby’s development.
To eat healthily, you should aim to do the following.
Most women do not need any extra calories during the first six months of pregnancy. It is only in the last 12 weeks that they need to eat a little more, and then only an extra 200 calories a day, which is roughly the same as two slices of bread.
What is a ‘healthy’ weight?
You can find out your healthy weight from your BMI (body mass index). This is a measure of your weight in relation to your height. Your healthcare team can work it out for you. A healthy BMI is above 18.5 but below 25. Being overweight carries risks for you and your baby (see the RCOG patient information Why your weight matters during pregnancy and after birth: information for you, which is available at: www.rcog. org.uk/womens-health/clinical-guidance/why-your-weight-matters-during-pregnancy-and-after-birth).
The more overweight you are, the greater the risks. Being underweight increases the risk of your baby not growing as well as he or she should.
Is it safe for me to diet while I am pregnant?
Trying to lose weight by dieting during pregnancy is not recommended as it may harm the health of your unborn baby. If you are concerned about your weight, your midwife can advise you and may refer you to a dietician.
Is it safe to eat fish while I am pregnant?
In general, eating fish is a healthy option during pregnancy, but the current advice from the Department of Health is to eat no more than two portions of oily fish, such as mackerel or salmon, a week. This is because too much of a substance found in oily fish (mercury) can be harmful to an unborn baby’s development.
Also, pregnant women should not eat more than two fresh tuna steaks or four medium-sized cans of tuna a week, and should avoid eating shark, swordfish or marlin.
I have been told not to eat liver while I am pregnant. Why?
Liver can contain high levels of vitamin A, which in high doses can harm the development of an unborn baby’s nervous system. It is rare for women in developed countries like the UK to be deficient in vitamin A so you should avoid eating foods such as liver and liver products like pâté.
Is it safe to eat peanuts while I am pregnant or breastfeeding?
You can eat peanuts or foods containing peanuts (such as peanut butter) while pregnant or breastfeeding. Eating peanuts does not appear to affect your baby’s chances of developing a peanut allergy. Don’t eat them if you’re allergic to them.
How can I reduce the risk of infection from food?
You can pick up some infections, such as listeria, salmonella or toxoplasmosis, from contaminated food. These can harm your unborn baby.
To reduce your risk of getting listeriosis:
To reduce your risk of getting salmonella:
Do I need extra vitamins (vitamin supplements) when I am pregnant?
Vitamins are needed for growth and development. There are 13 important vitamins: vitamins A, C, D, E and K and the vitamin B series. Apart from vitamin D, which we get from sunlight, most vitamins come from our diet. In the UK, it is quite common for people to be low in vitamin D and folic acid (vitamin B9). These vitamins are important in pregnancy and you can boost your levels by taking a vitamin supplement. Supplements of other vitamins are not usually advised since they may actually be harmful in pregnancy. The various vitamins and whether they are recommended in pregnancy are detailed below.
Vitamins that are recommended
Folic acid
Folic acid is one of the B vitamins and helps to reduce the risk of your baby having spina bifida.
Taking extra folic acid may also reduce the risk of heart or limb defects and some childhood brain tumours. The recommended daily dose is 400 micrograms (µg). Ideally, you should start taking extra folic acid before you conceive and continue to take it until you reach your 13th week of pregnancy. If you did not take folic acid before you became pregnant, start taking it as soon as you realise you are expecting a baby.
Some women take a higher dose of folic acid. Why?
If your risk of having a baby with spina bifida is higher than normal, you will be advised to take a daily dose of 5 milligrams (mg) of folic acid. This is higher than usual and it will need to be prescribed by a doctor. You may be advised to take an increased dose if:
Vitamin D
All pregnant women are advised to take a daily dose of 10 micrograms (µg) of vitamin D when pregnant and breastfeeding. This is because it is common in the UK for people to have low levels of vitamin D. Taking supplements can improve your baby’s growth during his or her first year of life, and can reduce their risk of developing rickets.
You are at particular risk of having low levels of vitamin D if:
If you are in one of these situations, you may be may be advised to take a higher daily dose of vitamin D.
When may I need extra vitamin K?
Vitamin K is needed for our blood to clot properly. Newborn babies have low levels of vitamin K, which puts them at risk of bleeding . To prevent this, you will be offered vitamin K for your baby after birth.
You do not need to take vitamin K supplements yourself during pregnancy unless it is thought that your baby is at particular risk of bleeding. This could be because you are taking certain medicines for epilepsy or if you have liver disease.
When may I need extra vitamin C?
Although routine supplements of vitamin C are not specifically recommended when you are pregnant, this vitamin helps iron to be absorbed. This may be of benefit during pregnancy, at a time when women are at risk of becoming anaemic.
Vitamins that are not recommended
There are many multivitamin tablets for use in pregnancy that contain a small amount of lots of vitamins. These are safe to take, but avoid taking large doses of the following vitamins unless a doctor prescribes them for a particular reason.
What about extra iron?
Most women do not need to take extra iron during pregnancy. Taking routine iron supplements will not necessarily benefit your health and may cause you unpleasant side effects such as heartburn, constipation or diarrhoea. Your midwife will check your blood at your booking appointment and at 28 weeks of pregnancy. You will only be advised to take iron if you are found to be anaemic or are at increased risk of becoming anaemic in pregnancy, for example if you are carrying twins.
Can I get help to buy vitamins?
If you are on certain benefits and/or are under the age of 18 years, help may be available to provide you with free supplements.
You can buy folic acid or pregnancy multivitamins from any pharmacy or supermarket. There is no evidence that expensive brands are any better than cheaper ones.
Where can I find out more information about healthy eating?
The following website can give you information about healthy eating before and during pregnancy and while breastfeeding:
NHS Choices – Your Pregnancy and Baby Guide: www.nhs.uk/conditions/pregnancy-and-baby/pages/pregnancy- and-baby-care.aspx#close.
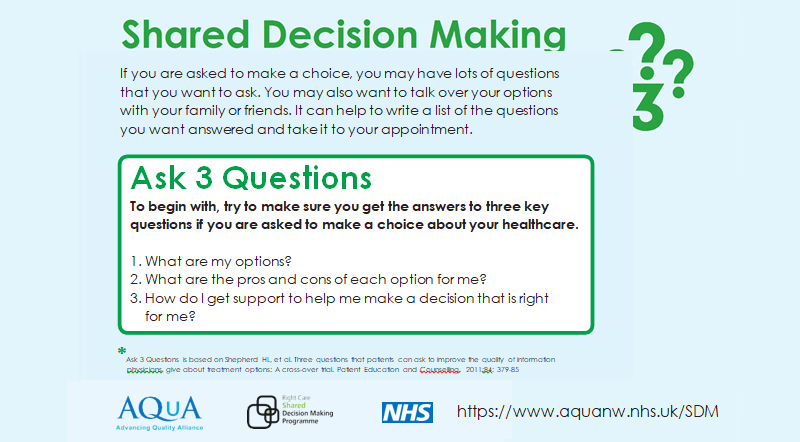
Making a choice
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on information from the NHS Choices website above and the RCOG scientific impact paper Nutrition in Pregnancy (September 2010; available at: www.rcog.org.uk/nutrition-pregnancy-sac-opinion-paper-18), which contains a full list of the sources of evidence we have used.
The RCOG produces guidelines as an educational aid to good clinical practice. They present recognised methods and techniques of clinical practice, based on published evidence, for consideration by obstetricians and gynaecologists and other relevant health professionals. This means that RCOG guidelines are unlike protocols or guidelines issued by employers, as they are not intended to be prescriptive directions defining a single course of management.
This information has been reviewed before publication by women attending clinics in London, Sheffield and Kirkcaldy.
A glossary of all medical terms is available on the RCOG website at: www.rcog.org.uk/womens-health/patient- information/medical-terms-explained.