Website maintained by Bageo Pharmaceuticals Pvt Ltd. All Rights Reserved
Who is this information for?
This information is for you if you wish to know more about endometriosis. It may also be helpful if you are the partner or relative of someone with endometriosis.
A glossary of all medical terms used is available on the RCOG website at: www.rcog.org.uk/en/patients/ medical-terms.
Key points
What is endometriosis?
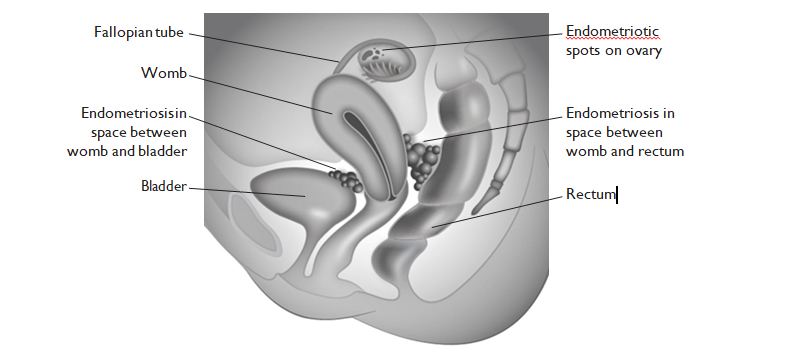
Endometriosis is a condition where tissue similar to the inner lining of the womb (endometrium) is found elsewhere, usually in the pelvis around the womb, ovaries and fallopian tubes. It is a very common condition, affecting around 1 in 10 women. You are more likely to develop endometriosis if your mother or sister has had it.
Endometriosis usually affects women during their reproductive years. It can be a long-term condition that can have a significant impact on your general physical health, emotional wellbeing and daily routine.
What are the symptoms?
Common symptoms include pelvic pain and painful, sometimes irregular or heavy periods. It can cause pain during or after sex and can lead to fertility problems. You may also have pain related to your bowels, bladder, lower back or the tops of your legs, and experience long-term fatigue. Some women with endometriosis do not have any symptoms.
Endometriosis can cause pain that occurs in a regular pattern, becoming worse before and during your period. Some women experience pain all the time but for others it may come and go. The pain may get better during pregnancy and sometimes it may disappear without any treatment. For more information, see the RCOG patient information Chronic (long-term) pelvic pain (www.rcog.org.uk/en/patients/patient- leaflets/long-term-pelvic-pain).
What causes endometriosis?
The exact cause of endometriosis is not known but it is hormone dependent. This means that, just like the endometrium which responds to hormonal changes resulting in a period, the endometrial-like tissue located outside the womb also bleeds. This bleeding can cause pain, inflammation and scarring, and can possibly damage your pelvic organs.
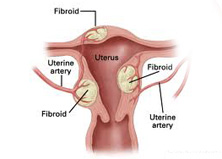
Endometriosis may be found:
Endometriosis can also occur within the muscle wall of the womb (adenomyosis) and occasionally on the bowel and/or bladder. It may sometimes be found in other parts of the body, but this is rare.
How is it diagnosed?
Endometriosis can be a difficult condition to diagnose. This is because:
See the section below on what tests may be offered to help diagnose endometriosis.
What will happen if I see a healthcare professional?
You should be asked:
Your GP may carry out an internal examination with your consent. This helps to localise the pelvic pain and the doctor can feel for any lumps or tender areas. You will be offered a chaperone during this examination. You will be able to discuss any concerns and you will have an opportunity to ask other questions.
Your GP may offer further tests, for example an ultrasound scan, and start treatment to help your symptoms. If your symptoms do not improve with the treatment offered or if you are unable to tolerate the treatment, your GP will refer you to a gynaecologist for further tests and treatment.
What tests might I be offered?
Tests usually include a pelvic ultrasound scan. This may be a transvaginal scan to check the uterus and ovaries. It may show whether there is an endometriotic (also known as a ‘chocolate’) cyst in the ovaries or may suggest endometriosis between the vagina and rectum.
You may be offered a laparoscopy, which is the only way to get a definite diagnosis. This is carried out under a general anaesthetic. Small cuts are made in your abdomen and a telescope is inserted to look at your pelvis. You may have a biopsy to confirm the diagnosis and images may be taken for your medical records.
Your healthcare professional may suggest treating the endometriosis at the time of your first laparoscopy, either by removing cysts on the ovaries or treating any areas on the lining of your pelvis. This may avoid a second operation. Sometimes, however, the extent of endometriosis found means that you may need further tests or treatment.
The procedure, including any risks and the benefits, will be discussed with you. After your operation you be will told the results. You can often go home the same day after a laparoscopy. For information about recovery following a laparoscopy, please see the RCOG patient information Laparoscopy (www.rcog.org.uk/ en/patients/patient-leaflets/laparoscopy).
An MRI scan may be suggested if the condition appears to be advanced.
What are my options for treatment?
The options for treatment include those listed below.
Pain-relieving medication There are several different medications to help relieve your pain. These can range from over-the-counter remedies to prescribed medications from your healthcare professional. In more severe situations, you may be referred to a specialist pain management team.
Hormone treatments These treatments reduce or stop ovulation (the release of an egg from the ovary) and therefore allow the endometriosis to shrink by decreasing hormonal stimulation.
Some hormone treatments that may be offered are contraceptive and will also stop you becoming pregnant. They include:
Other hormonal treatments are available but these are not contraceptives. Therefore, if you do not want to become pregnant, you will need to use a contraceptive as well. Non-contraceptive hormone treatments include:
SurgerySurgery can treat or remove areas of endometriosis. The surgery recommended will depend on where the endometriosis is and how extensive it is. This may be done when the diagnosis is made or may be offered later. Success rates vary and you may need further surgery. Your gynaecologist will discuss the options with you fully.
Possible operations include:
Sometimes other surgeons, such as bowel specialists, will be involved in your surgery. If you have severe endometriosis, you will be referred to an endometriosis specialist centre where a specialist team that could include a gynaecologist, a bowel surgeon, a radiologist and specialists in pain management will discuss your treatment options with you.
\Fertility treatmentGetting pregnant can be a problem for some women with endometriosis. Hormonal treatment is not advisable when you are trying to conceive and surgical treatment may be more appropriate. Your healthcare professional should provide you with information about your options and arrange timely referral to a fertility specialist if appropriate.
Other optionsSome women have found the following measures helpful:
Complementary therapiesAlthough there is only limited evidence for their effectiveness, some women may find the following therapies help to reduce pain and improve their quality of life:
Further information and support
National Institute for Health and Care Excellence (NICE) – Endometriosis: Diagnosis and Management:www.nice.org.uk/guidance/ng73
NHS Choices: www.nhs.uk/conditions/Endometriosis/Pages/Introduction.aspx
Endometriosis UK: www.endometriosis-uk.org
Fertility Network UK: http://fertilitynetworkuk.org/
British Society for Gynaecological Endoscopy: http://bsge.org.uk/
British Society for Gynaecological Endoscopy Accredited Centres: http://bsge.org.uk/centre/
RCOG Recovering Well series:
Laparoscopy: www.rcog.org.uk/en/patients/patient-leaflets/laparoscopy
Abdominal hysterectomy: www.rcog.org.uk/en/patients/patient-leaflets/abdominal-hysterectomy
Laparoscopic hysterectomy: www.rcog.org.uk/en/patients/patient-leaflets/laparoscopic- hysterectomy
Sources and acknowledgements